Naloxone India: A Promising Breakthrough with Patch and Wafer Solutions for Overdose Recovery
India is facing a growing opioid crisis, with overdose-related deaths becoming alarmingly frequent. In response, the healthcare community is turning its focus toward naloxone India—a life-saving drug that reverses the effects of opioid overdose. As government and non-government organizations like Prayas Sewa Samiti and various nasha mukti kendra in India explore best practices for deployment, a new question arises: should we use naloxone patches or naloxone wafers for maximum effectiveness and accessibility? This article provides a detailed comparison, exploring clinical data, field usage, benefits, and limitations to help rehab centers and healthcare professionals make informed decisions.
Addressing the Overdose Crisis with Naloxone India
What is Naloxone India, and why is it Critical?
Naloxone India refers to the locally available forms of naloxone being used or piloted for overdose reversal in both urban and rural Indian communities. Naloxone works by binding to opioid receptors and blocking the effects of drugs like heroin, fentanyl, or prescription opioids. The drug has been a global standard for emergency overdose response and is now gaining traction across Indian addiction recovery centers.
Naloxone India is particularly vital in:
-
Reducing fatal overdoses
-
Supporting harm reduction in high-risk zones
-
Empowering the nasha mukti kendra in India with emergency response tools
-
Increasing recovery success rates
The Two Delivery Systems: Patch vs Wafer
Naloxone Patch: A transdermal patch that slowly releases naloxone through the skin into the bloodstream. It’s often used as a preventive measure post-detox in supervised environments.
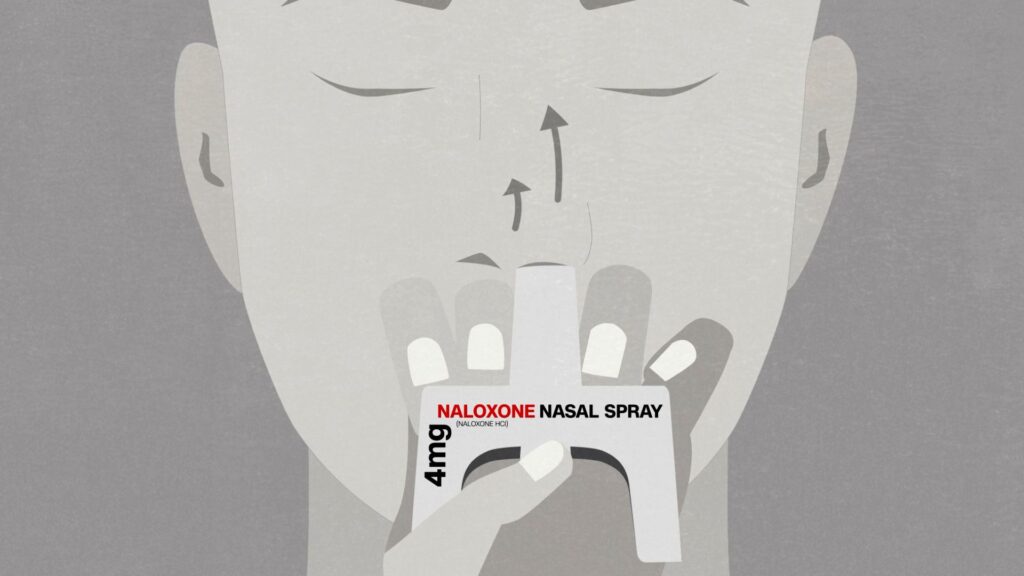
Naloxone Wafer: A rapidly dissolving oral strip or wafer placed under the tongue or in the cheek. It acts faster, making it suitable for emergency use during overdose events.
Efficacy and Onset Time: Which Works Faster?
Studies indicate:
-
Naloxone wafer takes effect within 2-3 minutes of administration.
-
Naloxone patch may take 15–30 minutes to reach therapeutic levels.
In urgent overdose cases, naloxone India solutions that offer faster onset—like wafers—are crucial. That’s why many emergency responders and nasha mukti kendra in India are leaning toward wafer deployment for field kits.

Accessibility in Indian Context: Logistics and Distribution
-
Patches require refrigeration and careful packaging to maintain potency, making them less ideal for rural distribution.
-
Wafers, in contrast, are compact, shelf-stable, and easy to administer even by laypersons after minimal training.
Organizations like Prayas Sewa Samiti are piloting wafer distribution in tier-2 and tier-3 cities due to these practical advantages.
Training and Administration: User-Friendliness
Naloxone India solutions must be easy to use. In field trials:
-
Wafers scored higher in ease of training for community health workers.
-
Patches require supervision, as the incorrect application can limit effectiveness.
This makes wafers more suitable for outreach programs and for use by family members in overdose-prone households.
Cost-Effectiveness: Budget Matters for Nasha Mukti Kendra in India
While naloxone India patches have a higher upfront cost due to technology and storage, wafers are:
-
Cheaper to produce
-
Easier to distribute in bulk
-
Less prone to misuse
This cost advantage is significant for underfunded nasha mukti kendras in India, many of which rely on NGO and government support like that offered by Prayas Sewa Samiti.
Side Effects and Safety Profile
Both naloxone delivery methods have a good safety profile. However:
-
Patches can cause skin irritation.
-
Wafers may lead to mild nausea or dizziness.
Neither poses a significant risk compared to the benefit of overdose reversal.
Integration with Nasha Mukti Kendra in India Protocols
Leading nasha mukti kendras in India are:
-
Stocking wafers in emergency kits
-
Offering training sessions on naloxone administration
-
Using patches for long-term relapse prevention in inpatient settings
Prayas Sewa Samiti has reported fewer relapses and quicker intervention in centers that integrate naloxone wafers into family counseling sessions and recovery planning.
Community Outreach and Public Awareness
Despite its effectiveness, naloxone India still suffers from a lack of awareness. Prayas Sewa Samiti and similar groups are launching:
-
Street plays and local campaigns
-
Poster drives in high-risk neighborhoods
-
WhatsApp-based educational videos
These efforts emphasize the difference between wafers and patches and guide communities on emergency response steps.
Regulatory and Policy Developments
The Drug Controller General of India (DCGI) is reviewing fast-track approvals for naloxone wafer manufacturing in India. Until now, most products were imported. Indigenous production will:
-
Lower costs
-
Improve availability
-
Boost local healthcare innovation
 Challenges in Deploying Naloxone India
Challenges in Deploying Naloxone India
-
Limited Rural Access: Many remote regions still lack access to basic healthcare, let alone overdose kits.
-
Stigma and Social Barriers: Opioid addiction is heavily stigmatized, which discourages families from keeping naloxone kits at home.
-
Training Gaps: Many nasha mukti kendras in India lack adequately trained staff to handle naloxone administration effectively.
-
Supply Chain Disruptions: Import dependency and storage issues can create bottlenecks in naloxone in India.
International Comparisons: What Can India Learn?
In countries like the U.S., Australia, and Canada, naloxone kits are available over the counter, and training is often given at schools, community centers, and even pharmacies. India’s path could benefit from:
-
Local manufacturing subsidies
-
NGO–NGO-government partnerships like that of Prayas Sewa Samiti
-
Regional language video training for rural populations
By adapting global best practices into the local context, naloxone India programs can be expanded more effectively.
Innovations Enhancing Naloxone India
-
Wearable Monitors: These trigger automated naloxone wafer releases if overdose symptoms are detected.
-
AI Prediction Models: Prayas Sewa Samiti is collaborating on projects that use AI to identify high-risk relapse situations where naloxone wafers may be necessary.
-
Educational Kits: Toolkits containing both wafer samples and training guides are being distributed in partnership with schools and community health centers.
Role of Media and Social Campaigns
Widespread awareness about naloxone in India requires ongoing public engagement. Campaigns are focusing on:
-
Featuring survivor stories
-
Myth-busting facts about naloxone side effects
-
Encouraging policy-makers to include naloxone wafers in standard emergency protocols

Integration into rural health programs
The Road Ahead: How Naloxone India Can Be Scaled
To meet the overdose crisis head-on, India needs to:
-
Prioritize funding for the mass production of naloxone wafers
-
Integrate naloxone education in school curricula
-
Provide incentives to the nasha mukti kendra in India that adopt best practices
-
Equip police stations and ambulances with wafer kits
Prayas Sewa Samiti recommends a “Naloxone for Every Home” campaign modeled on successful public health drives. Such initiatives could normalize carrying naloxone just as we do with first-aid kits or ORS packets.
Conclusion: Choosing the Right Tool in Naloxone India’s Battle Against Overdose
While both delivery forms of naloxone in India—patch and wafer—offer life-saving benefits, the wafer currently stands out as the preferred choice for emergency, low-resource, and wide-distribution contexts. Patches have their place in long-term relapse prevention but require closer supervision and infrastructure.
By incorporating naloxone wafers into everyday recovery plans, Nasha Mukti Kendra in India and partners like Prayas Sewa Samiti can empower families and communities to act swiftly during overdose crises.
Ultimately, the fight against addiction in India will be won not just through treatment, but through timely intervention, and naloxone India may be the most important tool in that mission.